Post-Traumatic Stress Disorder (PTSD) is a severe psychological condition that may develop after an individual is exposed to one or more traumatic events (Bisson et al., 2015)[1]. This article provides a comprehensive understanding of PTSD, delving into the symptoms, causes, diagnostic criteria, treatments, and real-life examples.
Understanding PTSD
PTSD can occur after experiencing or witnessing life-threatening events such as military combat, natural disasters, terrorist incidents, serious accidents, or violent personal assaults like rape (Kilpatrick et al., 2013)[2]. People who suffer from PTSD often relive the experience through nightmares and flashbacks, have difficulty sleeping, and feel detached or estranged (APA, 2013)[3].
Symptoms of PTSD
PTSD symptoms can be grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions (Shalev et al., 2017)[4].
Intrusive Memories include recurring, unwanted distressing memories of the traumatic event, flashbacks, nightmares, severe emotional distress or physical reactions to things that remind of the traumatic event (Friedman et al., 2011)[5].
Avoidance is the effort to avoid thoughts, feelings, or conversations about the traumatic event, places, people, or activities that remind you of it (APA, 2013)[6].
Negative Changes in Thinking and Mood include negative feelings about yourself or others, hopelessness, memory problems, difficulty maintaining relationships, lack of interest in activities, and feeling emotionally numb (Stein et al., 2012)[7].
Changes in Physical and Emotional Reactions (also called arousal symptoms) can include irritability, angry outbursts, always being on guard, overwhelming guilt or shame, self-destructive behavior, trouble concentrating or sleeping, and being easily startled (APA, 2013)[8].
Diagnosis of PTSD
PTSD is diagnosed by a mental health professional using the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which requires exposure to a traumatic event, presence of symptoms from all four symptom clusters, and symptom duration of more than a month causing significant distress or impairment (APA, 2013)[9].
Causes of PTSD
The development of PTSD can be influenced by the nature and intensity of the traumatic event, an individual’s response to it, and personal factors such as previous trauma exposure, family history of PTSD or depression, and personality traits (Breslau et al., 2010)[10].
Treatment of PTSD
Treatment for PTSD generally involves psychotherapy, medication, or a combination of both:
- Psychotherapy: Cognitive-behavioral therapy (CBT), exposure therapy, and eye movement desensitization and reprocessing (EMDR) are commonly used psychotherapeutic approaches (Cusack et al., 2016)[11].
- Medication: Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are often prescribed. Prazosin may be used to help reduce nightmares (Hoskins et al., 2015)[12].
Lifestyle Modifications and Self-care
Self-care strategies and lifestyle modifications play a significant role in managing PTSD. Regular physical activity, mindfulness practices, maintaining a strong support network, and following a balanced diet can help manage symptoms (Kearney et al., 2012)[13].
Real-Life Examples
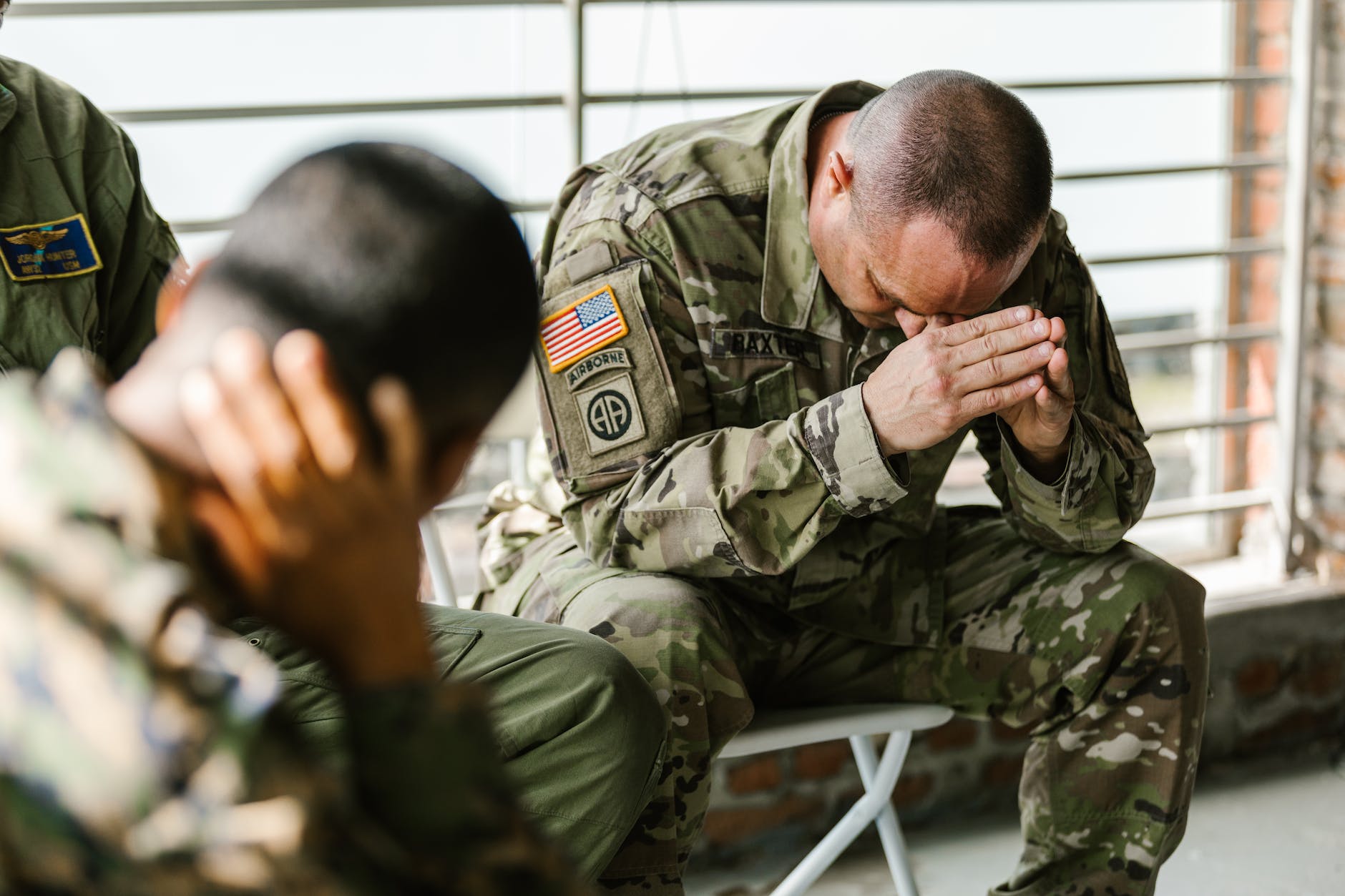
Understanding PTSD through real-life examples helps contextualize the disorder. For instance, a military veteran who served in a war zone may experience PTSD. Despite returning home safe, they could be plagued by flashbacks of combat, making them avoid situations that remind them of the trauma. They may also exhibit hypervigilance and have trouble sleeping due to nightmares of the event (Marmar et al., 2015)[14].
Another example could be a survivor of a severe car accident who continually relives the trauma, avoids driving or riding in cars, and experiences significant anxiety when near roads or hearing traffic sounds (Blanchard et al., 2004)[15].
Conclusion
PTSD is a debilitating mental health disorder that requires comprehensive and individualized treatment approaches. A profound understanding of this condition is necessary for effective diagnosis, treatment, and, ultimately, the improvement of the lives of individuals affected by it.
References
[1] Bisson, J. I., Cosgrove, S., Lewis, C., & Robert, N. P. (2015). Post-traumatic stress disorder. BMJ, 351, h6161.
[2] Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537-547.
[3] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
[4] Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-Traumatic Stress Disorder. New England Journal of Medicine, 376(25), 2459-2469.
[5] Friedman, M. J., Resick, P. A., Bryant, R. A., & Brewin, C. R. (2011). Considering PTSD for DSM‐5. Depression and Anxiety, 28(9), 750-769.
[6] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
[7] Stein, D. J., Koenen, K. C., Friedman, M. J., Hill, E., McLaughlin, K. A., Petukhova, M., … & Kessler, R. C. (2012). Dissociation in posttraumatic stress disorder: evidence from the world mental health surveys. Biological Psychiatry, 71(4), 4.
[8] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
[9] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
[10] Breslau, N., Koenen, K. C., Luo, Z., Agnew-Blais, J., Swanson, S., Houts, R. M., … & Moffitt, T. E. (2014). Childhood maltreatment, juvenile disorders and adult post-traumatic stress disorder: a prospective investigation. Psychological Medicine, 44(9), 1937-1945.
[11] Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., … & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128-141.
[12] Hoskins, M., Pearce, J., Bethell, A., Dankova, L., Barbui, C., Tol, W. A., … & Thornicroft, G. (2015). Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. The British Journal of Psychiatry, 206(2), 93-100.
[13] Kearney, D. J., McDermott, K., Malte, C., Martinez, M., & Simpson, T. L. (2012). Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology, 68(1), 101-116.
[14] Marmar, C. R., Schlenger, W., Henn-Haase, C., Qian, M., Purchia, E., Li, M., … & Ho, C. L. (2015). Course of posttraumatic stress disorder 40 years after the Vietnam War: Findings from the National Vietnam Veterans Longitudinal Study. JAMA psychiatry, 72(9), 875-881.
[15] Blanchard, E. B., Hickling, E. J., Forneris, C. A., Taylor, A. E., Buckley, T. C., Loos, W. R., & Jaccard, J. (1997). Prediction of remission of acute posttraumatic stress disorder in motor vehicle accident victims. Journal of Traumatic Stress, 10(2), 215-234.